Coxarthrosis affects the hip joints of middle-aged and elderly people. The causes of its formation are previous injuries, congenital and acquired inflammatory or non-inflammatory diseases. The leading symptoms of coxarthrosis are hip joint pain, morning swelling and stiffness in movement. In the initial stages of the pathology, the treatment is conservative. If coxarthrosis is ineffective due to rapid progression or late recognition, surgical intervention, usually endoprosthesis, is required.
Description of the pathology
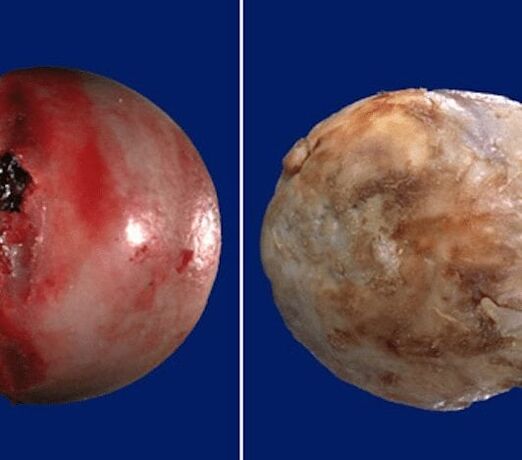
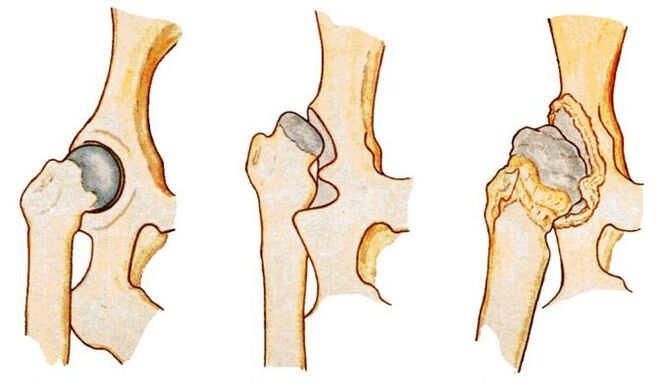
Coxarthrosis (osteoarthrosis, arthrosis deformans) is a degenerative-dystrophic pathology of the hip joint. In the initial stages of development, the structure of the synovial fluid changes. It becomes viscous and dense, which is why it loses its ability to nourish hyaline cartilage. As a result of dehydration, its surface dries out and is covered with multiple radial cracks. In this condition, the hyaline cartilage does not absorb shock well when the bones that make up the joint come into contact.
In order to adapt to the increased pressure on them, the bone structures are deformed by the formation of growths (osteophytes). The metabolism in the hip joint deteriorates, which negatively affects the muscles and ligaments of the joint.
degrees
Each stage is characterized by its own symptoms, the severity of which depends on the degree of narrowing of the joint space and the number of bone growths that have developed.
| Severity of coxarthrosis | Characteristic symptoms and radiographic signs |
|---|---|
| First | The joint space narrowed unevenly, single osteophytes formed around the acetabulum. Slight discomfort occurs, but more often the disease does not manifest itself clinically |
| Second | The joint gap narrows by almost 2 times, the head of the femur moves, deforms, enlarges, and bone growths are found outside the cartilage. Hip pain becomes constant and is associated with significant limitation of mobility |
| Third | Complete or partial fusion of the joint space, multiple bone growth, expansion of the femoral head. The pain occurs day and night and spreads to the thighs and legs. Movement is possible only with the help of a cane or crutches |

Causes of the disease
Primary coxarthrosis is a destructive-degenerative change in the hip joint, the causes of which have not been established. This means that the prerequisites for the early destruction of hyaline cartilage have not been identified. The following pathological conditions can provoke secondary coxarthrosis:
- previous injuries - fracture of the femoral neck or pelvic bones, dislocation;
- hip dysplasia;
- aseptic necrosis of the femoral head;
- congenital hip dislocation;
- inflammatory, including infectious diseases of the joint (rheumatoid, reactive arthritis, gout, tendinitis, bursitis, synovitis).
Prerequisites for the development of coxarthrosis are obesity, increased physical activity, sedentary lifestyle, metabolic disorders, hormonal disorders, kyphosis, scoliosis and flat feet.
Symptoms of the disease
In the initial stages of development, coxarthrosis can manifest itself only with mild pain. They usually appear after intense physical exertion or a hard day's work. The person attributes the deterioration of health status to muscle "fatigue" and does not seek medical help. This explains the frequent diagnosis of coxarthrosis in the 2nd or 3rd stage, when conservative therapy is ineffective.
Limitation of joint mobility
The range of motion of the hip joint decreases due to compensatory growth of bone tissue, damage to the joint membrane, and replacement of the joint capsule area with fibrous tissue that does not have functional activity. Mobility may be limited even in grade 1 coxarthrosis. Difficulties arise when rotating movements are performed with the legs.
As the disease progresses, morning stiffness and joint swelling become common. To restore mobility, a person needs to warm up for a few minutes. By lunch time, the range of motion is restored, among other things as a result of the production of hormone-like substances in the body.
Crunch
When walking, bending and (or) extending the hip joint, clicking, crunching and crackling sounds are clearly audible. The reason for the sound accompaniment of each step is the friction of bone surfaces, including osteophytes. Crackling can occur even in normal health due to the collapse of carbon dioxide bubbles in the joint cavity. Coxarthrosis is indicated by a combination of dull or sharp pain.
Pain
Painful sensations become permanent already in the 2nd stage of coxarthrosis. Their severity decreases somewhat after a long rest. The pain intensifies during the next relapse or the development of synovitis (inflammation of the joint membrane), which often accompanies osteoarthritis. In the remission phase, the discomfort decreases somewhat. But as soon as a person becomes hypothermic or lifts a heavy object, severe pain appears again.
Muscle cramp
Increased tension of the skeletal muscles of the thigh in coxarthrosis occurs for several reasons. First, the ligaments weaken. The muscles contract to hold the head of the femur in the acetabulum. Second, increased tone often accompanies inflammation of the synovial membrane. Third, when osteophytes are displaced, nerve endings are compressed and muscle spasm becomes a compensatory response to acute pain.
Lameness
In the later stages of the development of coxarthrosis, the patient limps severely. The change in gait is caused by flexion contractures and deformation of the bone surfaces, which makes it impossible to maintain a straight leg posture. The person also limps to reduce the severity of the pain by shifting their body weight to the unaffected limb.
Abbreviation for leg
Grade 3 coxarthrosis is characterized by a shortening of the leg by 1 cm or more. The reasons for the decrease in the length of the lower limb are severe muscle atrophy, thinning and flattening of the cartilage, narrowing of the joint space, and deformation of the femoral head.
Diagnostic methods
The initial diagnosis is made based on the patient's complaints, external examination, medical history and the results of several functional tests. Many inflammatory and non-inflammatory pathologies are disguised as symptoms of coxarthrosis, so instrumental and biochemical tests are performed.
X-ray examination
The stage of coxarthrosis is determined by X-ray examination. The resulting images clearly show the destructive changes in the hip joint. This is the narrowing of the joint space, the deformation of the bone surfaces and the formation of osteophytes.

CT scan
A CT scan is prescribed to patients to determine the degree of flattening and deformation of the hyaline cartilage. The results of the examination also enable the assessment of the condition of the ligament-tendon apparatus, nerve trunks, muscles, and the condition of young and old children.
Magnetic resonance imaging
MRI is one of the most informative studies in the diagnosis of coxarthrosis. In order to identify circulation disorders, contrast is used in the area of the affected joint. A routine examination is prescribed to determine the degree of ligamentous damage and deformation of the femoral head, as well as to detect areas of fibrous degeneration of the joint capsule.

Foot length measurement
Before the measurement, the doctor asks the patient to stand up and straighten his legs as much as possible. In order to obtain the most reliable data, the orthopedist uses two bones. Upper - the anterior axis of the pelvic bone, located on the anterior lateral surface of the abdomen at the outer edge of the inguinal ligament. The second reference point is any bony structure of the knee, ankle or heel. Measuring leg length is not necessarily informative if coxarthrosis affects two hip joints at the same time.
Laboratory research
Clinical blood and urine tests are performed to assess the general health of the patient. And the results of biochemical tests often make it possible to detect pathologies that cause the development of coxarthrosis. Gouty arthritis is indicated by high levels of uric acid and its salts. An increase in the sedimentation rate of erythrocytes and an increase in the number of leukocytes indicate the occurrence of an inflammatory process (bursitis, arthritis, synovitis). Rheumatoid factor, C-reactive protein and antinuclear antibodies are determined to rule out rheumatoid arthritis.

Hip puncture
Synovial fluid is collected by puncture to study its composition and detect changes in consistency. If an infectious-inflammatory process is suspected, further biochemical testing of the biological sample is warranted.
Treatment options
When determining the treatment tactics, the orthopedist takes into account the severity of the coxarthrosis, the form of its course, the causes of its development and the severity of the symptoms. Patients are often advised to wear a rigid rib bandage and orthosis from the first days of treatment. The use of orthopedic devices slows down the breakdown of cartilage and bone deformation.
Medicines
Medicines from various clinical and pharmacological groups are used in the treatment of deforming arthrosis. These are non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, glucocorticosteroids, chondroprotectors, ointments and warming gels.
Blockade
Intra-articular or peri-articular drug blockades are prescribed to relieve acute pain that cannot be removed with NSAIDs. Hormonal agents are used for their implementation. The analgesic effect of glucocorticosteroids is enhanced by their combination with anesthetics.
Injections
Intramuscular injection of NSAID solutions makes it possible to eliminate severe pain in the hip joint. A medicine is usually used to relax the skeletal muscles, which contains an anesthetic in addition to the muscle relaxant. In the form of injections, therapeutic treatments include B vitamins, drugs that improve blood circulation, and chondroprotectors.
Diet therapy
Overweight patients are advised to lose weight in order to slow down the spread of pathology to healthy joint structures. The calorie content of the daily menu should be limited to 2000 kilocalories, excluding foods high in fat and simple carbohydrates. Nutritionists recommend that all patients with coxarthrosis follow a proper diet. The diet should include fresh vegetables, fruits, berries, cereals, fatty sea fish and dairy products. The therapeutic diet strengthens the immune system and improves general health.
Exercise therapy and massage
Classical, acupressure and vacuum massage are used in the treatment of coxarthrosis. After several sessions, the blood circulation of the hip joint improves and the nutrient reserves are replenished. Carrying out massage procedures stimulates the strengthening of the ligament-tendon apparatus and the restoration of soft tissues damaged due to the displacement of osteophytes.
Regular exercise is one of the most effective ways to treat osteoarthritis. A series of exercises is put together by the physical therapist individually for the patient, taking into account their physical fitness.
Physiotherapy
Patients with coxarthrosis are prescribed up to 10 courses of magnetotherapy, laser therapy, UHF therapy, UV irradiation and shock wave therapy. The therapeutic effect of the procedures is due to improved blood circulation, acceleration of metabolism and regeneration processes. To relieve acute pain, electrophoresis or ultraphonophoresis is performed with glucocorticosteroids, anesthetics, and B vitamins. The use of ozokerite or paraffin helps to eliminate the discomfort.

Surgical intervention
If conservative treatment is ineffective, pain that cannot be eliminated by medication, or continuous progression of coxarthrosis, patients are advised to undergo surgery. Surgery is performed immediately in the case of pathology of the 3rd degree of severity, since the resulting destructive changes in the cartilage and bones cannot be eliminated by medication or exercise therapy.
Arthroplasty
The operation is performed under general anesthesia. The head of the femur is removed from the acetabulum. Visible destructive tissue changes are corrected - bone growth is removed, joint surfaces are smoothed, tissue that has undergone necrosis is excised. Cavities are created during the surgery and filled with ceramic implants.
Endoprosthesis
Hip replacement with an implant is performed under general anesthesia. In order to prevent the development of an infectious process, a course of antibiotics is prescribed. After 10 days, the sutures are removed and the patient is discharged from the medical facility. In the rehabilitation phase, patients are introduced to physiotherapy and massage treatments, as well as exercise.
Possible consequences
In the final stage of the pathology, flexion and adduction contractures develop. The patient's leg is constantly bent, so he uses a stick or crutches to move. After complete fusion of the joint space, immobility occurs, the patient cannot do housework and becomes disabled. Coxarthrosis is often complicated by aseptic necrosis of the femoral head, arthrosis of the knee joints, and arthritis.
Prevention and prognosis
Only grade 1 coxarthrosis responds well to conservative treatment. In other cases, endoprosthetics allow the complete restoration of the functional activity of the hip joint. After fitting the endoprosthesis, the patient quickly returns to an active lifestyle.
In order to prevent the disease, orthopedists recommend quitting smoking, abusing alcoholic beverages, daily physical therapy and gymnastics, and, if necessary, reducing excess weight.



































